Nebraska's #1 Trigger Finger Surgery Expert
Don’t let trigger finger hold you back. Whether you’re an athlete or simply struggling with everyday activities, finding the right trigger finger treatment is crucial. At Nebraska Hand & Shoulder, we are proud to be the state’s leading experts in Nebraska trigger finger surgery, offering advanced solutions to help you regain full mobility and live pain-free.
Our minimally invasive trigger digit release surgery is designed to effectively eliminate the root cause of your condition, providing lasting relief from pain and discomfort. From diagnosis to aftercare, our dedicated team will guide you through every step of the process, ensuring you receive the highest level of care.
Take the first step toward relief today. Contact us to schedule your appointment and learn more about our expert trigger digit surgery solutions.
Introduction To Trigger Finger
Do you feel pain or a popping sensation when bending your fingers? You might have trigger finger, a condition where inflamed tendons in the affected digit cause difficulty moving the finger or thumb. This can result in pain, tenderness, and even locking of the joint, making daily activities challenging. With proper diagnosis and treatment, you can ease symptoms and regain normal motion.
What Causes Trigger Finger?
Trigger finger happens when a tendon in your finger or thumb becomes irritated and thickened, restricting movement. This inflammation narrows the tendon sheath, leading to pain and the snapping or locking sensation during movement.
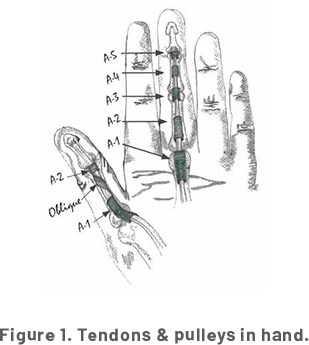
How Tendons and Pulleys Work
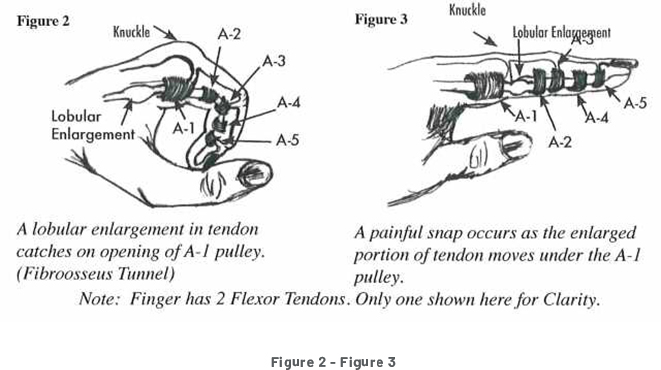
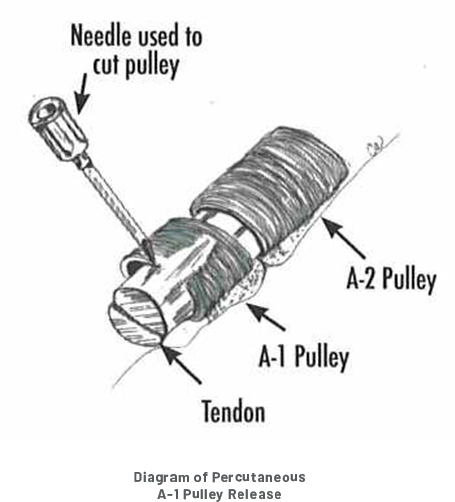
Tendons connect muscles to bones, allowing joint motion. They glide through channels supported by pulleys, which keep them in place. The A-1 pulley, often the problem site in trigger finger, can become thickened and restrict tendon movement, causing the snapping sensation.
Who’s at Risk?
Trigger finger is most common after age 30 and may be linked to genetics. While frequent use of the fingers hasn’t been proven to cause it, age and tissue changes are significant factors.
Symptoms of Trigger Finger
Discomfort and Tenderness
At the onset, a patient with trigger finger typically experiences localized discomfort in the palm of the hand at the palmar crease (knuckle level). Local tenderness and sometimes a nodule may be felt if the palm is pressed firmly.
Swelling and Stiffness of the Finger
In most patients, the involved finger or thumb feels swollen. Visible swelling, however, is the exception rather than the rule. One of the most common complaints of trigger finger is stiffness in the morning, which must be separated from possible arthritis. As the day wears on, the feeling of stiffness usually resolves.
Pain and Inability to Move
As the condition progresses, it becomes more painful, ultimately resulting in obvious snapping, getting to a point where one may have to manually straighten or bend the snapping finger with the other functioning hand. It can become too painful to move it through its own normal range of motion.
Triggering or Snapping
The most common triggering occurs in the thumb, second most commonly in the long finger. It can occur in all five digits, either simultaneously or one after the other. Actual triggering or snapping occurs due to the size difference between a tendon and its sheath (Figures 2 & 3).
Incidence
Trigger thumb occurs in 1 in 1000 infants. Due to an infant's tendency to clasp his thumb in a fist, congenital triggering is not usually picked up until after the sixth month of life. The majority of patients presenting with trigger finger are in their forties or fifties, and about 19% (1 out of 5) of patients have multiple digit involvement. Most adults with trigger digit have or have had carpal tunnel syndrome.
Treatment of Trigger Finger
At Nebraska Hand & Shoulder Institute, we specialize in advanced treatments for trigger finger to help you regain mobility and improve your quality of life. Don’t let the pain or discomfort of catching or locking limit you. Reach out today to learn more about our proven treatment options, including trigger finger release surgery performed by Dr. Ichtertz.
Early Treatment Options
Treating trigger finger early can increase the success rate of non-surgical options. While splinting to limit MP joint motion was once thought to help, studies show it’s ineffective since the issue isn’t caused by motion. Early treatment with steroid injections or anti-inflammatory medication may provide relief for some patients. However, the effectiveness of steroid injections varies, and while some experience lasting results, others may need additional treatment.
Late Treatment Options
For patients who have had symptoms for several months, severe catching or locking, or medical conditions like diabetes, steroid injections are often less effective. In these cases, surgical treatments are typically the best option. Minor trigger finger release surgery is performed to resolve the issue, especially for those with significant triggering or multiple affected digits. While injections may cause temporary discomfort, surgical options often offer a more permanent solution.
Trigger Finger Release Surgery: Why It’s Effective
When non-surgical options are not enough, surgical treatments can deliver excellent results. Dr. Ichtertz is a recognized expert in A-1 pulley release, an effective outpatient procedure that uses a small incision to relieve triggering. This minimally invasive technique involves low risk, minimal blood loss, and a shorter recovery time.
Most patients experience significant improvement after the procedure, with a high success rate. Risks are minimal but may include rare instances of infection or persistent tenderness.
Why Choose Nebraska Hand & Shoulder Institute?
Dr. Ichtertz and our team are dedicated to providing exceptional care tailored to your needs. Contact us today to schedule a consultation and take the first step toward relief with our advanced trigger finger treatments.
WARNING MAY CONTAIN GRAPHIC IMAGES

Prognosis
Some trigger digit patients go on to recover without the need for surgery. When surgery is undertaken, the prognosis is very good. A very small percentage of patients will continue to complain of local tenderness or pain.
Prognosis for A-1 Pulley Release
Dr. Ichtertz has a very successful track record with percutaneous trigger finger release. His failure rate is less than 1%. The failure rate for other surgeons was reported to be between 6 and 10 percent.
Contact Nebraska’s Top Trigger Finger Specialist
Do you suffer from a trigger finger and need relief? Look no further than Dr. Ichtertz, Nebraska's top specialist in treating trigger fingers. He is highly proficient in A-1 pulley release, which is a procedure that can be performed on an outpatient basis with minimal risk and no blood loss.
Although risks associated with this procedure are minimal, Dr. Ichtertz is highly experienced in managing any complications that may arise. Don't let a trigger finger impact your daily life any longer. Contact Dr. Ichtertz today to get the relief you deserve.
References
Anderson, Bruce Carl, et al, “Treatment of de Quervain’s tenosynovitis with corticosteroids.” Arthritis and Rheumatism, Vol. 34, No. 7, July 1991, pp. 793-798.
Badalamente, M.A., “Pathobiology of the Human A1 Pulley in Trigger Finger.” The Journal of Hand Surery, Vol. 16A, 1991, pp. 714-721.
Bishop, A.T., “Extensor Triggering in de Quervain’s Stenosing Tenosynovitis.” The Journal of Hand Surgery. Vol. 24A, 1999, pp. 1311-1314.
Dinham, J.M., Meggitt, B.F., “Trigger thumbs in children: a review of the natural history and indications for treatment in 105 patients.” Journal of Bone and Joint Surgery, Vol. 56B, No 1, 1974, pp. 153-155.
Doyle, J.R., Blythe, W.F., “The finger flexor tendon sheath and pulley: anatomy and reconstruction.” AAOS Symposium on Tendon Surgery in the Hand, St. Louis, 1975. The C.B. Mosby Company, pp. 81-87.
Doyle, J.R., “Anatomy of the Flexor Tendon Sheath and Pulleys of the Thumb.”, The Journal of Hand Surgery, Vol. 2, 1977, pp. 149-151.
Eastwood, D.M., Gupta, K.J., Johnson, D.P., “Percutaneous Release of Trigger Finger: An Office Prodedure.” Journal of Hand Surgery, Vol. 17A, 1992, pp. 114-117.
Ezaki, M., “Trigger Finger in Children.”, The Journal of Hand Surgery, Vol. 24A, 1999, pp. 1156-1161.
Fulcher SM, Hill, J.J.; “An Analysis of Patients with Multiple Trigger Digits.” [Poster] 56th Annual Meeting of the American Society for Surgery of the Hand Oct. 4, 2001, Seattle, WA.
Gray, R.G. and Gottlieb, N.L., “Hand flexor tenosynovitis in rheumatoid arthritis: prevalence, distribution, and associated rheumatic features.” Arthritis and Rheumatism, Vol. 20, No. 4, 1970, pp. 103-108.
Griggs, S.M., “Treatment of Trigger Finger in Patients with Diabetes Mellitus.” The Journal of Hand Surgery, Vol. 20, 1995, pp. 787-789.
Harvey, Francis J., et al, “deQuervain’s disease: surgical and non-surgical treatment.” Journal of Hand Surgery, Vol. 15A, No. 1, January 1990, pp. 83-87. (Diagram 4).
Hoffmann, R., “Open Versus Percutaneous Release of the A1-Pulley for Stenosing Tendovaginitis: A Prospective Randomized Trial.”, Techniques in Hand & Upper Extremity Surgery, Vol. 12, 2008, pp. 183-187.
Hollander, J.L., et al, “Hydrocortisone and cortisone injected into arthritic joints, comparative effects of and use of the hydrocortisone as a local anti-arthritic.” JAMA, Vol. 147, 1951, pp. 1629-1635.
Jackson, W.T., et al, “Anatomical variations of the first extensor compartment of the wrist: a clinical and anatomical study.” Journal of Bone and Joint Surgery, Vol. 68A, No. 6, July 1986, pp. 923-926.
Lane, L.B., “Commentary: Percutaneous Release of the First Annular Pulley.” The Journal of Hand Surgery, Vol. 20, 1995, pp. 785-786.
Lapidus, P.W., “Stenosing tenovaginitis.” Surgical Clinics of North America, Vol. 33, 1953, pp. 1317*1347.
Lubahn, J., “Complications of Open Trigger Finger Release.”, The Journal of Hand Surgery, Vol. 35A, 2010, pp. 594-596.
Medl, W.T., “Tendonitis, tenosynovitis, trigger fingers, and deQuervain’s disease.” Orthopaedic Clinic of North America, Vol. 1, No. 2, 1970, pp. 375-382.
Otto, N., Wehby, M., et al, “Steroid injections for tenosynovitis in the hand.” Orthopaedic Review, Vol. 15, No. 5, May 1986.
Patel, M.R., Bassini, L., “Trigger fingers and thumb: when to splint, inject or operate” Journal of Hand Surgery Vol. 17A, No. 1, Jan. 1992, pp. 110-113.
Patel, M.R., “Percutaneous Release of Trigger Digit With and Without Cortisone Injection.” The Journal of Hand Surgery, Vol. 22A, 1997, 150-155.
Peimer, C.A., “Release of the Sixth Dorsal Compartment.” The Journal of Hand Surgery, Vol. 19A, 1994, pp. 599-601.
Pratt, H.L., Bunnell, S., “Use of compound F (hydrocortisone in op) in operative and non-operative conditions of the hand.” Journal of Bone and Joint Surgery, Vol. 35, 1953, pp. 94-102.
Roth, J.H., “Percutaneous A1 Pulley Release: A Cadaveric Study.” The Journal of Hand Surgery, Vol. 20A, 1995, 781-784.
Sampson, S.P., et al, “Pathobiology of human A-1 pulley in trigger finger.” Journal of Hand Surgery, Vol. 16A, 1991, pp. 714-721.
Tanaka, J., “Percutaneous Trigger Finger Release.”, Techniques in Hand and Upper Extremity Surgery, Vol. 3, 1999, pp. 52-57.
Weilby, A., “Trigger finger: incidence in children and adults and the possibility of a predisposition in certain age groups.” Acta Orthopaedics Scandinavia, Vol. 41, 1970, pp. 419-427.
Weiss, A.C., “Treatment of De Quervain’s Disease.” The Journal of Hand Surgery, Vol. 19A, 1994, pp. 595-598.
Witczak, J.W., “Triggering of the Thumb with de Quervain’s Stenosing Tendovaginitis.” The Journal of Hand Surgery, Vol. 15, 1990, pp. 265-268.
Witt,J. “Treatment of de Quervain Tenosynovitis: A Prospective Study of the Results of Injection of Steroids and Immobilization in a Splint.” Journal of Bone & Joint Surgery, Vol. 73, 1991, pp. 219-222
Woods, T.H.E., “deQuervain’s disease: a plea for early operation: a report on 40 cases.” British Journal of Surgery, Vol. 51, No. 5, May 1964, pp. 358-359.