Shoulder Arthritis Treatment in Nebraska
Persistent shoulder pain, especially during movement or after a long day, requires a thorough evaluation. At Nebraska Hand & Shoulder Institute, we utilize advanced X-ray technology and comprehensive physical exams to identify the root causes of your shoulder pain, such as arthritis, shoulder impingement, carpal or cubital tunnel syndrome, or, in rare cases, tumors.
Getting an accurate diagnosis is crucial for effective treatment of shoulder arthritis. Explore our specialized surgical and treatment services for shoulder arthritis below, or contact us today to schedule an appointment and take the first step toward relief.
Understanding Shoulder Arthritis
Within the shoulder, two areas may be affected by arthritis: the main glenohumeral joint and the acromioclavicular (AC) joint. Pain from the AC joint is usually localized to the top of the shoulder and is often exacerbated by arm movements away from the body, known as abduction. In contrast, arthritis in the glenohumeral joint typically leads to a loss of motion and increased pain in all directions, particularly during rotation toward and away from the body.

Who Gets Shoulder Arthritis
Shoulder arthritis can affect a wide range of individuals, particularly as they age. Degenerative arthritis occurs when cartilage cells fail to maintain themselves, leading to erosion of the joint cartilage. This erosion creates a surface that resembles a moon crater and eventually results in complete cartilage loss, causing bone-on-bone contact. The combination of pain and the loss of a normal gliding surface leads to a decrease in joint mobility.
In cases of rheumatoid arthritis, the body essentially attacks itself, inflicting damage on the joints with inflammatory substances. Total shoulder joint replacement is often necessary for patients with this condition. Additionally, untreated rotator cuff tears can result in a deterioration of the joint, known as "cuff-tear arthropathy."
By the time individuals reach an age where degenerative shoulder arthritis (DJD) may develop, they might already be experiencing arthritis in the cervical spine (neck). Research from the University of Pennsylvania indicates that MRI scans reveal signs of acromioclavicular (AC) joint degeneration in approximately 70% of asymptomatic volunteers by the age of 40. In contrast, x-ray evidence of DJD takes much longer to manifest.
Carpal tunnel syndrome and cubital tunnel syndrome commonly affect adults over 30, with women being five times more likely to experience these conditions than men. It is relatively rare for patients to present with shoulder pain as their primary or sole complaint due to nerve entrapment; often, these individuals may also have significant cervical disc degeneration, complicating the evaluation process. As a result, one or more overlapping issues may coexist, making diagnosis and treatment more challenging.


Treatment for Shoulder Arthritis
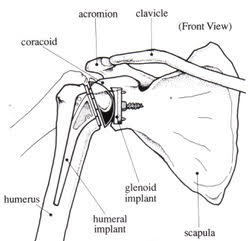
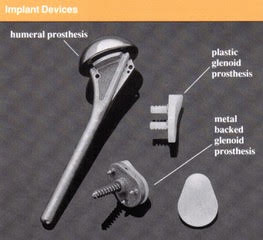
Shoulder joint replacement has evolved alongside advancements in hip and knee replacements over the past 40 years. The implants utilize the same high-density metal and polypropylene materials for their surfaces. Currently, approximately 50,000 total shoulder joint replacements are performed annually in the United States.
Total shoulder replacement (TSA) is an option for individuals with arthritic shoulders who do not respond to non-steroidal anti-inflammatory medications (NSAIDs) or who are intolerant to them. Below, you'll find a diagram and an X-ray illustrating a TSA procedure.
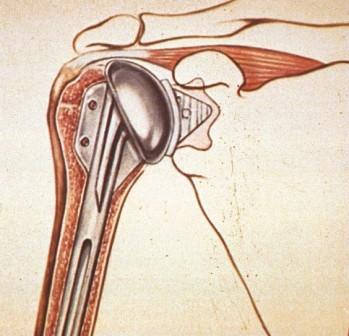
TSA Diagram

X-Ray
Reverse Total Shoulder Arthroplasty
Reverse total shoulder arthroplasty (RTSA) is a surgical procedure that enables the deltoid muscle to become the primary driver for arm elevation when the rotator cuff is non-functional. Although the arm may appear slightly unnatural post-surgery, patients often find relief from pain, which tends to outweigh aesthetic concerns.

Introduction and General Information
Reverse total shoulder arthroplasty was introduced to the US market in 2003.
The lever arm of the deltoid muscle is almost double with a reverse prosthesis, thus, the efficacy of the deltoid for abduction of the shoulder is also approximately doubled. However, it negatively affects the active external rotation. Also with RTSA, the deltoid muscle fibers that are under tension when the arm is at one's side (adduction) undergo much more shortening during a given arc of abduction (arm away from the side) and begin to lose strength beyond approximately 80 to 90 degrees. This is the effect of changing the center of rotation inferiorly and medially (towards the chest wall).
Optimizing Treatment for Proximal Humeral Fractures: RTSA vs. Hemiarthroplasty
Three- and four-part fractures of the upper end of the humerus, known as proximal humeral fractures, are most effectively treated with reverse total shoulder arthroplasty (RTSA). This approach offers a more reliable return to function compared to attempts at repairing the tuberosity through hemiarthroplasty, which often proves ineffective, with more than 40% of cases resulting in nonunion. In younger patients, there is a greater tendency to opt for hemiarthroplasty over reverse total shoulder arthroplasty.
When it comes to acute three- and four-part upper humerus fractures, patients tend to recover more readily after RTSA than after partial shoulder replacement (hemiarthroplasty), as the former procedure does not require meticulous protection and rehabilitation. Typically, these patients regain overhead elevation, although they may experience limited external rotation.
With RTSA, outcomes are generally moderate—neither excellent nor extremely poor—while hemiarthroplasty can yield excellent results if the tuberosities heal correctly. Conversely, poor outcomes are common when the greater tuberosities fail to heal, occurring in about 40% of cases, as noted in the article by Gerber C., Pennington SD., and Nyffeler R., published in JAAOS, May 2009, Vol. 17, No. 5, pages 284-295.

Risks and Complications
Reverse total shoulder arthroplasty has been shown to have about a three-fold increased complication rate over a primary shoulder arthroplasty. There is evidence that results depend on the indication for which RTSA is used in the first place. For massive rotator cuff tear arthropathy (massive CTA), at four years 90% of patients were very satisfied or satisfied in the French 484-patient, multi-center study. At 10 years postop in the study of Mole, 89% of the prostheses were still in place with 72% of patients with a high score.
For rheumatoid arthritis (RA), it is essential to make sure there is adequate glenoid bone stock. Studies have shown that there is deterioration of results over 5 to 10 years in this group of patients.
Infection: Deep infection has been shown to occur in 5% of primary cases of RTSA in France (Mole D. and Favard L. reference in 2007). This is possibly because of the large dead space created for blood collection after surgery. Component loosening (glenoid) when it occurs involves about 4-7% of glenoid components with risk factors of younger patient age, i.e. less than 70, and female sex.
Instability: Instability occurred in about 3% of the Mole study. When this occurs a year or more after surgery it can usually be successfully treated by closed reduction, i.e. without actually opening up the shoulder.
For more information on shoulder pain related to carpal tunnel syndrome you may review the following article:
Kummel, B.M., Zazanis, G.A. "Shoulder pain as the presenting complaint in carpal tunnel syndrome." Clinical Orthopaedics, May 1973; 92:227-230.
Take Control of Your Shoulder Health Today!
Don't let shoulder pain hold you back any longer. At Nebraska Hand & Shoulder Institute, our team is dedicated to providing you with a comprehensive approach to diagnosing and treating shoulder arthritis. Whether it's through advanced imaging, targeted therapies, or surgical options, we are here to help you regain your mobility and quality of life. Contact us today to schedule your appointment and take the first step toward a pain-free future!