Ulnar Wrist Pain
Suffering from chronic pain at the outer edge of your wrist? This could be ulnar-sided wrist pain, an uncomfortable condition that requires accurate diagnosis and treatment for long-term relief. At Nebraska Hand and Shoulder Institute, our lead orthopaedic surgeon, Dr. Ichtertz, and his skilled team are experts in understanding and treating ulnar wrist pain.
This type of wrist pain, also known as pain on the pinkie finger side, can be triggered by multiple factors. Recognizing the root cause and delivering the right diagnosis is paramount to creating an effective treatment plan. Our dedicated team at the Nebraska Hand and Shoulder Institute is skilled in diagnosing and providing solutions that will significantly reduce or even eliminate your chronic ulnar wrist pain.
Why suffer when you can get professional wrist pain treatment in Omaha, Lincoln, and Grand Island, Nebraska? Contact us today to schedule an appointment and embark on your journey to a pain-free life.
Understanding Ulnar Wrist Pain
The ulna is the smaller of the two bones of the forearm, located on the same side as the small finger. Pain on the ulnar side of the wrist is relatively common in adults, though not in children. This issue is seen most commonly in men in their late twenties to forties, often following a fall on an outstretched hand, with or without an associated broken bone.
Taking a careful history, performing a thorough examination, and providing treatment skillfully can lead to a cure or significant improvement in the majority of cases. Advances in arthroscopic surgical technique and wrist research over the past decade have played a key role in achieving these positive outcomes.
Derangement in the wrist often leads to pain, reduced grip and pinch strength, and may affect sleep. Overall, it results in a loss of productivity.
Anatomy
The wrist, or carpus, is composed of eight bones working together as one unit, plus the ends of the two forearm bones - the radius and the ulna. Wrist motion occurs in four directions: up (dorsal), down (palmer), or side-to-side (radial and ulnar).
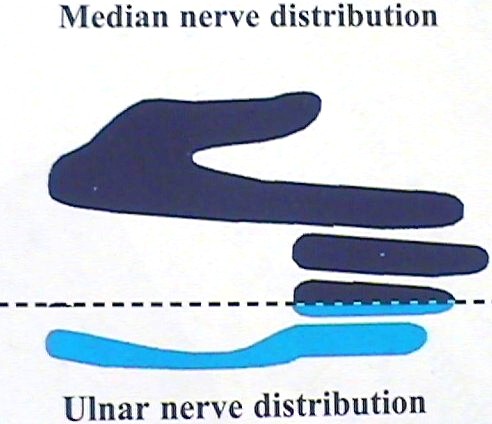
The radial half of the wrist is predominantly supplied with sensibility from the median, superficial radial, and posterior interosseous nerves while the ulnar side of the wrist is usually innervated from the ulnar nerve. Thus, entrapment of the ulnar nerve at the wrist, or more commonly at the elbow, may result in ulnar wrist or ulnar hand pain and/or burning, numbness, aching and decreased tolerance for writing or other manual activities.
Differential Diagnoses & Causes
1) Ulnar Tunnel Syndrome
Symptoms of numbness and burning, clumsiness, and pain in the ulnar side (small finger side) of the hand usually occur at the same time as the symptoms on the opposite side of the hand; i.e. the same time as a person with carpal tunnel syndrome. To a large extent, it is a moot point except when it comes to excluding ulnar nerve entrapment at the cubital tunnel. This is because carpal tunnel release simultaneously decompresses the ulnar nerve in Guyon's canal. Guyon's canal ( the ulnar tunnel) is directly adjacent to the carpal tunnel, separated by a septum.
As far as I can discern, the relief of the symptoms occurs much like the relief experienced by a person sitting in the front seat of a bench-type car seat when extra occupants beyond the normal two leave; i.e. when three or four are sitting on the seat designed for two passengers, there is much more space available for the remaining passengers when the couple of those squeezed in are allowed to leave.
When we open up the carpal tunnel, we are widening it. According to research done on CT and MRI scans, we are increasing the size of the carpal tunnel by about 25% and eliminating the pressure. It is extremely uncommon to have to perform isolated ulnar tunnel decompression; i.e. ulnar tunnel syndrome as an isolated entity does not occur very often and when it does, we need to be wary of a possible ganglion in the canal.
It is also unnecessary to separately open up the ulnar tunnel at the time of carpal tunnel release surgery. This has been well established in the medical literature. Richman and Gelberman* in 1989, on the basis of what appeared to be quite a limited study, concluded that ulnar nerve decompression at the time of carpal tunnel release occurred because of the change in the shape of Guyon's canal with the decompression; i.e. it changed from a trapezoid to more of an oval, providing relief.
I have seen many MRI scans of patients pre- and post carpal tunnel release for other reasons, and I have yet to see a configuration similar to that which they published in their article. I do not believe that their specific interpretation (change in shape from a trapezoid to an oval) is as likely as the one I have indicated above.
Pressure on the ulnar nerve causing the muscle to spasm.

No pressure on the ulnar nerve.
2) Cubital Tunnel Syndrome
Cubital tunnel syndrome, or entrapment of the ulnar nerve at the elbow, occurs in about three women for every man. Usually patients are over age 30. It also tends to occur almost exclusively in a person who sleeps with his or her elbow bent (flexed).

Improper Sleep Posture
3) Torn Triangular Fibrocartilage (TFCC)
A torn TFCC is diagnosed by local TFCC tenderness on the top of the wrist. Ulnar wrist pain tends to worsen with movement of the hand to the direction of the ulna (ulnar deviation), gripping, twisting and pounding often causes increased symptoms. Confirmation is with a positive arthrogram or direct visualization during arthroscopy (most accurate). MRI scanning may possibly show a torn TFCC, but we have less experience with the MRI and it is a more expensive test. Swelling indicates synovitis - engorgement of the joint or tendon lining.
Outcome of Surgery for Torn TFCC
| Procedure | Surgeon | Outcome |
| Arthroscopic Trimming | Melone 1991 | 83% Good/Excellent |
| Osterman 1990 | 88% Good/Excellent | |
| Ulnar Shortening | Melone 1998 | 92% Good/Excellent |
| Hulsizer 1997 | 91% Excellent |

Example of normal TFCC

Example of torn TFCC
4) Kienbock's
Kienbock's is a term applied to painful loss of blood supply (bone infarct) occurring in the lunate of the wrist. There is no good explanation why it occurs. Fortunately, it is relatively rare.
Though there are numerous treatment options, overall satisfaction is about 70%, i.e. there is room for improvement. Unloading of the lunate and/or reestablishing blood flow by insertion of an artery or a bone block with an artery attached are the main options in early disease before the lunate crumbles. After bone crumbles then salvage procedures such as PRC or fusion are available.

Bone appears more solid due to loss of blood flow causing it to die and crumble.
5) Ulnocarpal Abutment
Ulnocarpal abutment causes pain from impact of the prominent ulna on the wrist bones. It results from incorrect healing of a wrist fracture in which the ulna is left longer (relative to the radius) than it had been before the injury. Degenerative growth disturbance may also cause this. Thus the prominent ulna also crushes the TFCC.
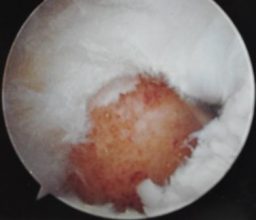
End of trimmed ulna as seen through hole in TFCC


6) Ulnar Artery Thrombosis (Hypothenar Hammer Syndrome)
Ulnar artery clotting occurs predominantly in heavy smokers, over age 50, who also do a lot of pounding with their hands. These patients usually present with finger tip lesions.

Finger tip ulcer at different stages of healing after circulation cut off by tiny clots

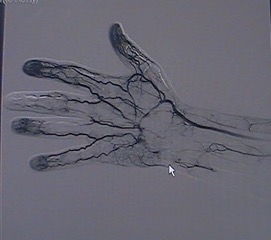
Arthrogram showing blocked ulnar artery
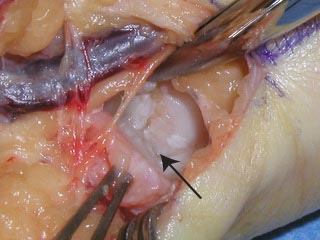
7) Ganglion Cyst
A ganglion cyst is a small fluid-filled degenerative sac protruding from a joint or tendon sheath; these occur frequently on the wrist. They occasionally cause pain. Surgical removal is the treatment of choice though about 15% will recur.

8) Piso-Triquetral Arthritis
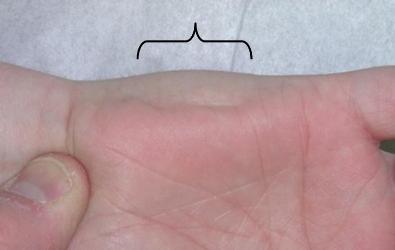
Pisotriquetral arthritis is an uncommon small joint degenerative arthritis occurring between the pisiform and the triquetrum. The pisiform really is essentially an extra bone. It doesn’t do much of anything and the best treatment for this problem is just to remove the pisiform which doesn’t hurt much and is very effective in relieving all of the discomfort.
If a person is suffering degenerative arthritis elsewhere in their body, NSAID may be taken to treat all of the areas simultaneously and, if that doesn’t eliminate the pain adequately, then the pisiform can be removed. Patients whose x-ray is included here for illustration underwent removal of the pisiform with complete elimination of their pain and minimal discomfort.

9) Extensor Carpi Ulnaris Tendinosis
It is unclear exactly why it develops. It is analogous to the very common de Quervain’s tendinosis which occurs almost exclusively in women in the thumb side of the wrist with the first extensor compartment tendons.
The extensor carpi ulnaris muscle is very important in lifting the wrist up and tilting it to the ulnar side of the hand, the most functional position for the hand. It is a fairly powerful muscle. In the past, tendinosis of the extensor carpi ulnaris at the wrist was, in my experience, quite rare.
In the last few years I have been seeing a few cases a year and it is treated with cortisone injection initially and if that doesn’t resolve it within a few days a minor operation through about a 1-inch incision on the top of the wrist as an outpatient eliminates the pain very quickly. No postoperative immobilization is necessary. There is minimal scar.
There may be some mild decreased sensitivity in the skin just beyond the incision for a few weeks to a few months in some cases because of the dorsal cutaneous branch of the ulnar nerve, which is in the general area and sometimes has to be pulled to the side to protect it during the procedure. This problem does not appear to be any more common in laborers vs. sedentary, stay-at-home people vs. office workers.
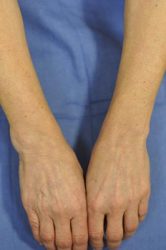
Note the swelling in the exterior of the wrist on the left
10) Carpal Instability (Lunotriquetral Instability)
There are eight bones directly within the wrist joint and those connect with the two bones in the forearm, the radius and ulna, and the metacarpal bones in the hand. On the ulnar side of the wrist, between the lunate and the triquetrum, a rare form of instability known as lunatotriquetral instability may develop.
This typically occurs in response to trauma falling on the wrist and disrupting the ligaments to the joint. Once the diagnosis is confirmed with x-ray, MRI and/or wrist arthroscopy, fusion of the lunatotriquetral joint is the best treatment.


Advanced Ulnar Wrist Pain Treatment in Nebraska
At the Nebraska Hand & Shoulder Institute, we offer specialized treatment for ulnar wrist pain, tailored to the unique needs of each patient. Whether you're in Omaha, Lincoln, or Grand Island, Nebraska, you can rely on our professional services to provide the relief you need.
Our treatment approach begins with a thorough examination. We localize the site of maximum discomfort and use advanced diagnostics, including x-rays and MRI scanning if needed. If there's suspicion of avascular necrosis, our MRI scan could be key in ruling it out.
For issues like a torn ligament, we may employ arthrography (dye injection study) or arthroscopy, which provides a more accurate assessment. Depending on your specific condition - whether it's due to degeneration, trauma, or nerve entrapment - we'll formulate a personalized wrist pain treatment plan.
Ulnar wrist pain treatment often involves trimming the Triangular Fibrocartilage Complex (TFCC) for most types of tears. Our experienced surgeon, Dr. Ichtertz, carries this out using an outpatient arthroscopic technique; a procedure involving several small punctures in the wrist, through which a fiberoptic scope and tools are inserted.
Alternatively, treatment may involve shortening of the ulna bone for abutment syndrome. This procedure entails removing a small wedge of bone from the ulna and stabilizing it with a metal plate and screws. With the secure fixation, patients usually won't need a cast during the 8 to 12-week healing process.
In cases of degenerative arthritis or instability within the wrist, limited carpal fusion may be the preferred treatment. This procedure binds two or more of the eight wrist bones together to limit pain-causing motion. Furthermore, Proximal Row Carpectomy (PRC) is an increasingly popular option due to its effectiveness in allowing retention of motion.
With over a decade in orthopaedic practice, Dr. Ichtertz is adept in diverse strategies for chronic ulnar wrist pain treatment. Trust Nebraska Hand & Shoulder Institute for effective solutions for ulnar wrist and ulnar sided wrist pain.

Proximal Row Pre-Op

Proximal Row Post-Op
Risks of Surgery
Most wrist operations cause little pain and all are performed on an outpatient basis. Every operation has inherent risks: a remote risk of infection, nerve injury, and new or increased pain are possibilities. An attempt at wrist fusion may result in non-union, i.e. non-healing, especially in smokers, thus may require a second operation in a rare case. Of course with any operation there are some people who develop prominent scars. This occurs more often and is more noticeable in people with a dark complexion.
Schedule Your Wrist Pain Appointment Today
Ulnar wrist pain can be complex and challenging to both diagnose and manage. However, our lead surgeon, Dr. Ichtertz, excels in accurately diagnosing and effectively treating this type of discomfort, whether it's chronic ulnar wrist pain or out wrist pain.
Our approach to treating ulnar wrist pain prioritizes non-surgical methods whenever possible. We utilize anti-inflammatory and analgesic medications, splinting, and injections to alleviate your discomfort and address the underlying issue. We don't believe that physical therapy is always the most beneficial solution for hand or wrist pain, nor do we consider work absences as part of our treatment plan.
Our ultimate goal at Nebraska Hand and Shoulder Institute is to keep you productive. We strive to provide treatments that allow for maximum hand function.
Don't let your ulnar sided wrist pain hold you back. Schedule your appointment at the Nebraska Hand & Shoulder Institute today and take your first steps towards a pain-free life.
Allan CH, Joshi A, Lichtman DM: Kienböck’s disease: diagnosis and treatment. Am Academy Ortho Surg 2001; 9:128-136.
Bain GI, Pugh MW, MacDermid JC, Roth JH: Matched hemiresection interposition arthroplasty of the distal radioulnar joint. J Hand Surg 1995; 20A:944-950.
Begley BW, Engber WD: Proximal row carpectomy in advanced Kienböck’s disease.
Chidgey LK: The distal radioulnar joint: problems and solutions. J Am Acad Ortho Surg 1995; 3:95-109.
Constantine KJ, Tomaino MM, Herndon JH, Sotereanos DG: Comparison of ulnar shortening osteotomy and the wafer resection procedure as treatment for ulnar impaction syndrome. J Hand Surg 2000; 25A:55-60.
DiBenedetto MR, Lubbers LM, Coleman CR: Long-term results of the minimal resection Darrach procedure. J Hand Surg 1991; 16A:445-450.
Hulsizer D, Weiss A-PC, Akelman E: Ulna-shortening osteotomy after failed arthroscopic debridement of the triangular fibrocartilage complex. J Hand Surg 1997; 22A:694-698.
Kirschenbaum D, Coyle MP, Leddy JP: Chronic lunotriquetral instability: diagnosis and treatment. J Hand Surg 1993; 18A:1107-1112.
Minami A, Kato H: Ulnar shortening for triangular fibrocartilage complex tears associated with ulnar positive variance. J Hand Surg 1998; 23A:904-908.
Osterman AL: Arthroscopic debridement of triangular fibrocartilage complex tears. J Arthro Related Surg 1990; 6(2):120-124.
Palmer AK: Triangular fibrocartilage disorders: injury patterns and treatment. J Arthro Related Surg 1990; 6(2):125-132.
Palmer AK, Werner FW, Glisson RR, Murphy DJ: Partial excision of the triangular fibrocartilage complex. J Hand Surg 1988; 13A;403-406.
Palmer AK, Werner FW: The triangular fibrocartilage complex of the wrist - anatomy and function. J Hand Surg 1981; 6(2):153-162.
Pin PG, Young VL, Gilula LA, Weeks PM: Management of chronic lunotriquetral ligament tears. J Hand Surg 1998; 14A:77-83.
Richman JA, Gelberman RH, Rydevik BL et al. Carpal tunnel syndrome: morphologic changes after release of transverse carpal ligament. J Hand Surg 1989; 14A:852-857.
Shin AY, Sheetz KK, Bishop AT, Berger RA: Vascularized pedicled bone grafts from the distal radius: technique and results of treatment for scaphoid nonunion and Kienböck’s disease. Mayo Clinic 1997.
Simmons SP, Tobias B, Lichtman DM: Lunate revascularization with artery implantation and bone grafting. J Hand Surg 2009; 34A:155-160.
Tomaino MM: The importance of the pronated grip x-ray view in evaluating ulnar variance. J Hand Surg 2000; 25A:352-357.
Watanabe T, Takahara M, Tsuchida H, Yamahara S, Kikuchi N, Ogino T: Long-term follow-up of radial shortening osteotomy for Kienböck’s disease. JBJS Am 2008; 90:1705-1711.